Introduction
Neuropilin 1 (NRP1) is one of two homologous neuropilins (NRP)
expressed in all vertebrates that has important physiological and
pathological roles.1 It was identified first in 1987 by Takagi and his coworkers as a neuronal receptor in developing Chick nervous system.2 NRP1 can exist in two isoforms, namely, secretory and transmembrane isoforms.3,4
The former, also known as truncated or soluble NRP1, circulates freely
in the body fluid, whereas the latter isoform, transmembrane NRP1, is a
highly conserved single-pass transmembrane protein that interacts with
different ligands and has multifaceted functions, including mediating of
varieties of physiological and pathological processes; as a result, it
is commonly called NRP1.1,3,4
Since its emergence in December 2019, the 2019 coronavirus disease
(COVID-19) pandemic, caused by novel severe acute respiratory syndrome
coronavirus 2 (SARS-CoV-2), has been severely challenging the global
healthcare systems, economies, and social life.5
COVID-19 is primarily a disease of the respiratory tract typically
transmitted from person to person through respiratory droplets and
direct contact with SARS-CoV-2 infected individuals or inanimate
objects. It is highly infective and transmissive compared to SARS-CoV,
as it usually spreads rapidly via active pharyngeal viral shedding.6–8
The global threat of COVID-19 urgently demands extensive efforts to
develop vaccines and antiviral therapies that curb the global spread and
impact of COVID-19. Thus, growing our extensive knowledge regarding
SARS-CoV-2 entry mechanisms is central for designing COVID-19 therapies
and vaccines. The entry of SARS-CoV-2 to the host cells requires binding
with the host receptors via the viral protein called spike (S) protein.9 Besides ACE2 and CD147, recently, a novel receptor called NRP1 was identified for SARS-CoV-2 entry to the host cell.10,11 Hence, this minireview presents the role of NRP1 in SARS-COV-2 entry and as a possible therapeutic target.
Overview of SARS-CoV-2 Entry Mechanism
It is the virus–host cell interactions that determine the cellular entry of SARS-CoV-2 and its dissemination across the tissues.12
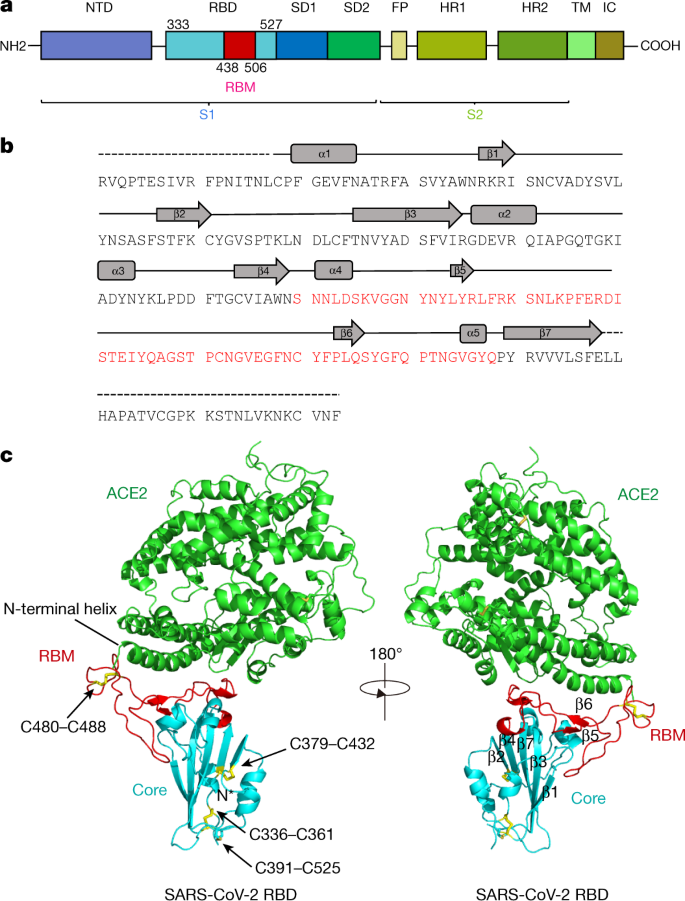
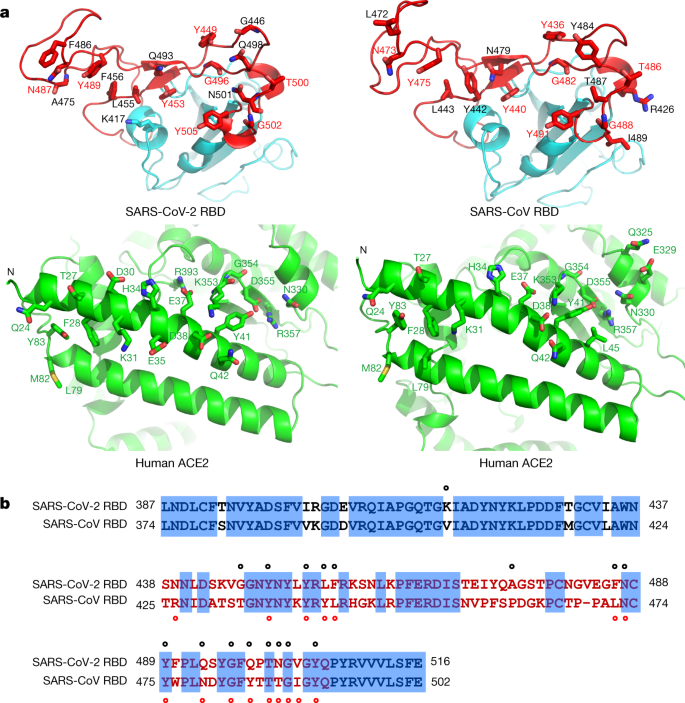
To infect humans, like SARS-CoV, the S protein of SARS-CoV-2 must first
bind to surface receptors of human cells lining the respiratory or
intestinal tracts. Once attached, the virus invades the cell then
replicates multiple copies of itself. The copies of viruses are then
released and lead to the SARS-CoV-2 transmission.12,13
The process of viral attachment to and invasion of human cells occurred using different
cellular receptors. Several studies on SARS-CoV-2 entry have so far
been carried out mainly on ACE2 and have confirmed that, like SARS-CoV,
the S protein of SARS-CoV-2 uses ACE2 as a host surface receptor to
enable the virus to enter and infect the cell.10,14–19
In addition to ACE2, CD147 protein has been identified as a co-receptor
in host cells to enhance the ability of SARS-CoV-2 to enter human
cells, and cause COVID-19 disease.11,14,16,17,20,21
In spite of these entry mechanisms, it was not clearly understood why
the tissue tropism of SARS-CoV-2 varies from what is expected from
virus–host cell interaction via ACE2 receptor, and why SARS-CoV-2
readily infects tissues other than the respiratory system, such as the
brain, heart, and other tissues with no or low ACE2 expression. These
raised the possibility that other host factors are required to
facilitate virus–host cell interactions in cells with low ACE2 protein
level.6,22
Thus, some studies were recently conducted to reveal these unclear
mechanisms, and intriguingly, a major breakthrough study by Daly et al
as well as a genetic based study by Cantuti-Castelvetri et al and Li and
Buck identified a novel receptor called NRP1 that potentially answer
the puzzling question what makes SARS-CoV-2 highly infectious and
capable of rapidly spreading in human cells.6,22,23
They concluded that NRP1 may serve as an alternative or independent
doorway for SARS-CoV-2 entry to and invasion of the human cells.
The Structure and Ligands of Neuropilin 1
NRP1, formerly known as A5 protein, is a 120–140 kDa non-tyrosine
kinase multifunctional transmembrane heptameric protein with an ATWLPPR
sequence consisting of 923 amino acids.1
It is encoded by the NRP1 gene located on the 10p11.22 human chromosome
locus and shares 44% amino acid sequence identity with its homology,
NRP2.3,4,24
NRP1 comprises a large N-terminus extracellular domain, a relatively
very small plasma membrane spanning transmembrane domain, and a short
cytoplasmic tail in the inner side of the cell membrane. The
extracellular domain in turn comprised of three different subdomains,
namely A, B, and C subdomains (Figure 1).1,3
The A or a1-a2 subdomains, also called semaphorin (SEMA) binding
subdomains, are located on amino end and contains two complement binding
motifs (CUB), namely the complement binding components (C1r and C1s),
Uegf (urchin embryonic growth factor), and bone morphogenetic protein 1
(BMP1), whereas the B subdomain involving b1-b2 subdomains are found in
the middle of the extracellular domain and are characteristics of
clotting factor V and VIII, and discoidin proteins.25–27
This domain is also known as the vascular endothelial growth factors
(VEGF) binding subdomain as it serves as a binding site for VEGF.1
The third domain, called C domain, has similarity with MAM (Meprin,
A5/NRP1, protein tyrosine phosphatase μ and К) and contributes for homo-
or hetero-dimerization of other receptors with the transmembrane
domain, thereby affecting distinct downstream signaling cascades.3 The transmembrane domain is a single-pass protein consisting of a conserved GXXXG repeat crossing the cell membrane.27–29
A short domain of NRP1 that contains 43–44 amino acids but lacks
tyrosine kinase activity is the cytosolic tail. This domain possesses a
PDZ-binding motif that can interact with various proteins such
RGS-GAIP-interacting protein (GIPC) and synectin that are essential for
via VEGF receptor 2 (VEGFR2) signaling, arterial morphogenesis as well
as in maintaining the structural integrity of transmembrane proteins.1,3,27
 |
Figure 1 Schematic diagram of NRP1
Structure. NRP1 contains a large N-terminus extracellular domain
comprising A (a1-a2), B (b1-b2), and C subdomains, a very small
single-pass plasma membrane spanning TM domain, and a short cytoplasmic
domain in the inner side of the cell membrane possessing PDZ-binding
motif that can interact with various proteins. The a1/a2/b1 segment
binds with SEMA3s, VEGFs, and other proteins, and the C domain involved
in receptor dimerization with the TM domain. The b1 of NRP1 binds with S
protein of SARS-CoV-2 and facilitate infection. Abbreviations: NRP1, neuropilin 1; SEMA3s, class 3 semaphorin family; TM, transmembrane; VEGFs, vascular endothelial growth factors.
|
Although it lacks a direct cellular signaling role, NRP1 is most
widely known for its crucial role as a multifunctional co-receptor by
forming a complex with other membrane receptors to form holoreceptors.1
Numerous previous studies have shown that NRP1 is a membrane protein
that serves as a surface receptor that can bind with wide varieties of
protein families, including heparin-binding members of the VEGF family,
class 3 members of the SEMA family (SEMA3s) such as SEMA3A, 3C, and 3F,
transforming growth factor-β1 (TGF-β1).28,30,31
The SEMA3s are well known to bind to the a1/a2/b1 portion, whereas the
VEGFs bind to b1/b2 segments of NRP1. In addition, NRP1 has recently
been demonstrated to act as a receptor for extracellular microRNAs,
fibroblast growth factor 2 (FGF-2), galectin-1, hepatocyte growth factor
(HGF), plexin, β1 integrin, epidermal growth factor (EGF),
platelet-derived growth factor (PDGF), hedgehog (Hh), and other growth
factors, albeit their binding sites are not well characterized.32,33
Furthermore, a small portion of S protein is currently recognized to
be complementary with the b1 domain of human NRP1 protein and allows the
binding of SARS-CoV-2 to host cells and hence facilitate infection.6,22
The Role of Neuropilin 1 in Health and Disease
Many studies have pointed out that NRP1 is broadly distributed in the
tissues of the human body, with a predominant expression in blood
endothelial cells, vascular smooth muscle cells, mesenchymal stem cells,
retinal vasculature, neurons, and epithelial cells lining the
respiratory and gastrointestinal tracts.1,3,6,22,24
NRP1 has been established to play a myriad of physiological,
pathological, and therapeutic roles. As indicated by the plethora of
evidence, NRP1 has versatile functions in regulating a wide array of
biological processes, such as axon guidance within the central and
peripheral nervous systems, angiogenesis, vascular permeability, and
cell survival, proliferation, differentiation, migration, and invasion.2,3,30,32
In recent years, NRP1 has also been shown to be expressed by various
immune cells, such as macrophages, including alveolar, adipose tissue,
bronchial, and vascular macrophages, dendritic cells, T-cells,
particularly CD8 cells, regulatory T-cells, B-cells, and mast cells
where it controls a multitude of functions, including development,
migration, and recruitment, communication between different immune
cells, as well as immune system regulation under normal physiological
condition.3,4
NRP1 has also been detected in bone cells like osteoclasts and
osteoblasts where it has an important role in regulating bone
remodeling, for instance osteo-protection through its binding with
SEMA3A.3,34,35
Besides, many other studies have improved the understanding of the
roles of NRP1 in different pathological conditions, including cancer,
immunological disorders, and bone diseases though the molecular
mechanisms behind these functions are still to be elucidated.3,33,34
NRP1 is generally overexpressed in various clinical disorders,
including malignancies, where it upregulates the oncogenic activities of
malignant cells by enhancing cell survival and proliferation, and
angiogenesis, as well as by contributing therapeutic resistance.1,3,33
Moreover, NRP1 has been investigated to have a potential role as a
therapeutic target in various pathological disorders, for instance in
cancer it serves as an antiangiogenic target as well as in cancer and
autoimmune diseases it acts as a site for immunotherapies but it needs
selective targeting of NRP1 under a particular clinical setting.3,33
Intriguingly, recent encroaching studies have unveiled an additional
role of NRP1 in COVID-19 infection, which was found to be a cofactor and
facilitator of SARS-CoV-2 entry and could pave the way to a new
possible target of intervention for COVID-19.6,22 More recently, an NRP1 receptor was reported in one study as a potential new target for pain inhibitors to treat chronic pain.36
This discovery is based on the grounds of the pain-relieving activity
of SARS-CoV-2, which is suggested to mediate the interactions of NRP1
with S-protein by preventing the normal binding of a protein called
VEGF-A to NRP1 and blocking pain signals to give pain relief. However,
before developing analgesics, more research is required on how NRP1
contributes to pain signaling.
Neuropilin 1 and COVID-19
Neuropilin 1 Mediated SARS-CoV-2 Entry Mechanism
According to recent studies, NRP1 is identified as a novel
co-receptor as well as a potentiating factor for SARS-CoV-2 entry
process by enhancing the interaction of the virus with ACE2 (Table 1).6,22,23,37 Daly et al suggested that it may act as an alternative doorway for SARS-CoV-2 to enter and infect human cells.22
Consistently, the study by Cantuti-Castelvetri et al using tissues from
human autopsies revealed that NRP1 significantly potentiates SARS-CoV-2
infectivity.6
Furthermore, this study demonstrated that the NRP1 is expressed
strongly in respiratory and olfactory epithelia, while the ACE2 is
absent or expressed at low level and hence it may provide an independent
gateway for viral entry and invasion of the host cells. Thus, the NRP1
may mediate SARS‑CoV‑2 entry into the brain via the olfactory bulb.6
In agreement with this, a study by Davies et al showed NRP1 is
expression in the CNS, involving olfactory‑related regions such as the
olfactory tubercles and para-olfactory gyri, suggesting the potential
role of NRP1 as an additional mediator of SARS‑CoV‑2 infection
implicated in the neurologic manifestations of COVID-19.37
Moreover, one review article has also suggested that the brainstem has a
relatively high expression of ACE2 receptor, and possibly NRP1, that
SARS-CoV-2 exploits for cell infection. Thus, the respiratory,
cardiovascular, gastrointestinal, and neurological functions of the
brainstem may be compromised indefinitely as a result of brainstem
damage manifested with neurological symptoms even in mild cases of
COVID-19 and may results in long-lasting consequences.38
Their abundant expression on epithelia exposed to the external
environment as well as their multifaceted functions are the possible
reasons that make NRP1 an ideal entry factor for SARS-CoV-2 as well as a
critical contributing factor for multisystem involvement of SARS-CoV-2
infection.4,6,22
 |
Table 1 A Summary Table on the Role of NRP1 in SARS-CoV-2 Infection
|
SARS-CoV-2 uses a small piece of S protein located on the outer
surface of the virus to attach to a complementary region of NRP1
receptors on human cells and hence to penetrate the host cells (Figure 2).6 The cell entry phase of SARS-CoV-2 depends on priming of S protein by host cell proteases.39,40
At the S1/S2 boundary, there is a multi-basic sequence motif called
RRAR containing arginine (R) and alanine (A) amino acids, with a
sequence of Arg-Arg-Ala-Arg. The RRAR amino acid sequence is a unique
feature of SARS-CoV-2 that provides a cleavage site for a host
proprotein convertase (furin) and possibly form additional cell surface
receptor binding sites and thus enhances pathogenicity by priming the
fusion activity.39–41
This is confirmed by another study demonstrating that SARSCoV-2 virus
with a natural deletion of the S1/S2 furin cleavage site is associated
to attenuated pathogenicity in hamster models.42
 |
Figure 2 The potential NRP1 mediated
SARS-CoV-2 entry mechanism into human cells. The trimeric S protein of
SARS-CoV-2 binds to host ACE2 via RBM of RBD. Furin mediated cleavage of
S protein at S1/S2 site exposes the CendR motif of S1 and enables
binding to the b1 subdomain of NRP1. Further processing of S protein by
TMPRSS2 on the cell surface (early entry pathway) and CTSL in
endolysosome (late entry pathway) exposes the FP and triggers membrane
fusion, and the viral RNA get into the host cytoplasm. The genomic RNA
undergoes replication and translation to form new SARS-CoV-2 virions
after assembly in ERGIC and the new viruses finally released into the
outside of the cell. Abbreviations:
ACE2, angiotensin converting enzyme 2; CendR, C-end rule; CT,
cytoplasmic tail; CTD, C-terminal domain; CTSL, cathepsin L; FP, fusion
peptide; HR, heptad repeat; NRP1, neuropilin 1; NTD, N-terminal domain;
RBD, receptor binding domain; RBM, receptor binding motif; TM,
transmembrane domain; TMPRSS2, TM serine protease 2; ERGIC, endoplasmic
reticulum–golgi intermediate compartment.
|
The furin protease cuts the full-length S protein into S1 and S2
functional polypeptides and forms a multi-basic RRAR sequence on the
carboxyl-terminal of S1 polypeptide. Studies based on x-ray
crystallography and biochemical approaches have shown that the S1 C-end
rule (CendR) motif is known to directly interact to b1 domain of NRP1 by
electrostatic attraction and activate the cell surface receptors.4,6,22
However, even though the CendR peptide of S1 domain is a major
recognition site for NRP1, it is not yet known which other segments of
NRP1 and the S protein may interact. In addition, a comparable binding
between the carboxy-terminal sequence of S1 subunit and NRP1 homolog,
NRP2, was also demonstrated.22
A more recent study by Zhenlu and Matthias also indicated that NRP1
facilitate SARS-CoV-2 infection by stimulating the separation of S1 and
S2 subunits.23
This study modeled the structures of NRP1 a2/b1/b2 binding to S protein
of SARS-CoV-2 and showed NRP1 on binding with S protein trimer bound to
an ACE2 dimer. The S1 binds more strongly to the host membrane in the
presence of NRP1 and destabilizes the S1/S2 interface and hence
increases the likelihood of the S2 subunit to be pulled out rather than
S1 being stretched. Thus, NRP1 attachment may stimulate the easier
dissociation of S2 from the S1 subunit that triggers membrane fusion
and, thus, increase virus infectivity.23
Following the binding of ACE2 and NRP1 with S1 of SARS-CoV-2, further
processing of S protein by transmembrane serine protease 2 (TMPRSS2) on
the cell surface (early entry pathway) and cathepsin L(CTSL) in
endolysosome (late entry pathway) occur. This exposes the fusion peptide
(FP) that triggers membrane fusion, and the viral RNA get into the host
cytoplasm. Then the genomic RNA undergoes replication and translation
to form new virions after assembly in ERGIC, and the new viruses then
are released into the outside of the cell.43,44
Previous studies showed that NRPs are known to mediate the
internalization of CendR ligands through an endocytosis resembling
micropinocytosis but it is unclear whether NRP1 allows attachment and
receptor-mediated endocytosis in SARS-CoV-2 infected patients.6,22,45,46 Thus, further studies need to be done to clearly explain the role of NRP1 in the entry and infection mechanisms of SARS-CoV-2.